I can vividly remember being taught how to ‘scrub up’ as a third-year medical student. The careful scrutiny of the theatre sister filled me with fear. Had I touched the wrong part of the scrub pack? Were my hands completely sterile? On more than one occasion I completely forgot to put on my facemask and had to start again from scratch. The consultant surgeon rapidly lost patience with my ineptitude… ‘Barton, what the hell are you doing?! Get in here and hold this retractor now!’
There is something almost ritualistic about the whole experience. The mantra that aseptic technique saves lives is one of the very first things learnt by medical students. The prevention of the spread of harmful organisms is far better than dealing with potential sepsis caused by poor hygiene. It saves countless lives on a daily basis in hospitals all around the world.
It all seems so obvious now, but as hard as it is to imagine this wasn’t always the case. In fact, there was a time when it was considered to be positively unseemly to wash your hands if you were a physician, the mere suggestion that you should causing great offence. This might still be the case today if it weren’t for the work of Ignaz Semmelweis.
Ignaz Semmelweis was born to a wealthy family on July 1st, 1818 near Budapest in Hungary. He initially studied Law at the University of Vienna before switching to Medicine in 1838. He completed his medical training in 1844 and subsequently decided to specialise in obstetrics, being appointed as an assistant on a maternity ward at the Allgemeines Krankenhaus (General Hospital) in Vienna in 1846.

Semmelweis was appointed to work on a maternity ward at Vienna General Hospital in 1846.
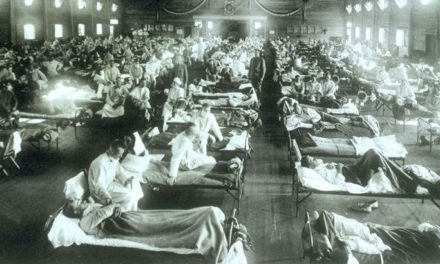
In the mid-1800s deaths from puerperal infections, at the time referred to as ‘childbed fever’, were commonplace. A puerperal infection is any infection of the female reproductive tract occurring after childbirth, usually a bacterial infection of the uterus. The most commonly implicated bacteria are Streptococcal spp. and Staphylococcal spp. Even today these can spread to the bloodstream and cause septicaemia, and with no antibiotics available then death was frequently the outcome.
Semmelweis quickly became interested in these puerperal infections and in particular the dramatic difference in death rates between the two different maternity divisions that operated at the Allgemeines Krankenhaus for the two different classes of patients. In the first division, to which he had been appointed, the deliveries were carried out by medical students and physicians. In the second division, the deliveries were carried out by midwives. He observed that women in the first division had a 13-18% rate of post-delivery mortality compared with only a 2% rate in the second division. There surely had to be an explanation for this vast difference?
In the mid-1800s the germ theory of disease had not yet been established and the miasma theory was still strongly supported. Miasma theory held that disease was spread by a poisonous form of ‘bad air’ that was emitted from rotting organic matter. It was something of a mystery as to why such a difference in mortality rates should be occurring.

A representation of miasma theory by the artist Robert Seymour.
Semmelweis’ first observation was that women in the first division gave birth on their sides, whilst women in the second division gave birth on their backs. Perhaps this was could be the reason for the differing mortality rates? He decided to change practice and had the women in the first division also give birth on their backs. This resulted in no change in the mortality rates.
His next observation was that a priest would walk through the ward of the first division ringing a bell following a death. This didn’t happen in the second division. Semmelweis hypothesized that the priest must have terrified the women so much that they subsequently developed a fever and died. He made the priest abandon the bell ringing and change his route. Once again there was no change in the mortality rates. At this time Semmelweis was starting to become frustrated with his failure to isolate the cause of the discrepancy in the mortality rates.
It was at this point that something very important occurred. A close friend of Semmelweis, a pathologist called Jakob Kolletschka, had cut himself with a scalpel blade whilst performing an autopsy on a patient who had died of childbed fever. Kolletschka became unwell and subsequently died from ‘cadaveric fever’. It was thought that miasma from the corpse had been transferred to him. Death in this manner for pathologists was a common occurrence at this time. Semmelweis studied his friend’s case and came to the crucial realization that he had died suffering the exact same symptoms as those of childbed fever. Kolletschka’s death had provided him with a vital clue.

A painting of a 1800s autopsy by the artist Enrique Simonet.
Autopsies were commonly performed at this time and it was standard practice for medical students and physicians to handle corpses immediately before proceeding directly to the wards to treat patients or perform deliveries. Semmelweis suspected that ‘putrid particles’ from these autopsies were getting onto their hands and being transferred to the obstetric wards and that this was responsible for the increased infection rates in the first division. He decided to test this hypothesis with a study that instituted hand washing using a chloride of lime solution before deliveries. Mortality rates in the first division fell immediately to 2%, the same as in the midwife-led division. Spurred on by his discovery he decided to wash the medical instruments used as well. This time the mortality rate dropped further to only 1%. The case was closed, hand washing should become standard practice, or so it would seem.
Semmelweis’ superior, Professor Johann Klein, disagreed with his findings and opposed his institution of hand washing. He supported the theory that the hospital’s new ventilation system was transmitting miasma and causing the childbed fever cases. He refused to renew Semmelweis’ assistant professorship and, feeling betrayed, Semmelweis left Vienna and returned home to Budapest.

Semmelweis, aged 42 in an 1860 copperplate engraving by Jenő Doby
In 1851 Semmelweis was appointed the head of obstetrics at St. Rochus Hospital, where he continued his work on hand washing and also successfully reduced maternal mortality rates. In 1855 he became a professor at Pest University, where he once again managed to reduce maternal mortality rates.
Later, in 1861 he published the book, ‘The Etiology, Concept, and Prophylaxis or Childbed Fever’, but it received a number of unfavourable reviews and was widely criticised. By this time he was becoming markedly embittered by the opposition to his work and findings. Following these reviews, he lashed out against his critics in a series of open letters that were full of bitterness and desperation.

Semmelweis’ 1862 Open Letter to all Professors of Obstetrics
His conduct became increasingly erratic and sources state that he was becoming an embarrassment to his colleagues. By 1865 he was drinking heavily and his behaviour worsened, being described as irrational, odd, and inappropriate. He was spending more and more time away from his family and began to frequent prostitutes.
There is considerable debate as to the exact cause of his behavioural changes. It has been suggested that he may have been suffering from Alzheimer’s disease or that perhaps he had tertiary syphilis. It may simply be that the constant criticism and ridicule that his life’s work received drove him mad. Later that year he was committed to a Viennese insane asylum. He was only an inpatient for two weeks but during that time he endured severe beatings, was secured in a straightjacket, doused with cold water, and administered castor oil as a laxative. He died on August 13th, 1865 from a gangrenous wound that was possibly caused by one of his beatings. In an ultimate ironic twist, his cause of death was given as pyaemia, he had died from sepsis aged only 47.
Semmelweis was buried in Vienna in August 1865, having received no recognition in his own lifetime for his work on the prevention of disease transmission. Another 20 years would pass until his work was revisited and he finally received credit. By 1880, following work by Louis Pasteur and Robert Koch, the miasma theory was largely abandoned, the germ theory of disease established and the value of hand washing truly appreciated. Long after his death Semmelweis would be remembered as the ‘Saviour of Mothers’. The term ‘the Semmelweis reflex’ is used as a metaphor for ‘the reflex-like tendency to reject new evidence or new knowledge because it contradicts establish norms, beliefs or paradigms’.
It is perhaps best to finish this remembrance of Semmelweis with a quote by the man himself from his final hours: “When I look back upon the past, I can only dispel the sadness which falls upon me by gazing into that happy future when the infection will be banished … The conviction that such a time must inevitably sooner or later arrive will cheer my dying hour.”




Recent Comments